High quality clinical documentation is more than a procedural requirement—it is an essential part of delivering safe, consistent, and person-centred care. For therapists, having a structured way to capture assessments, treatments, and clinical reasoning not only strengthens professional practice but also ensures better continuity of care for every client.
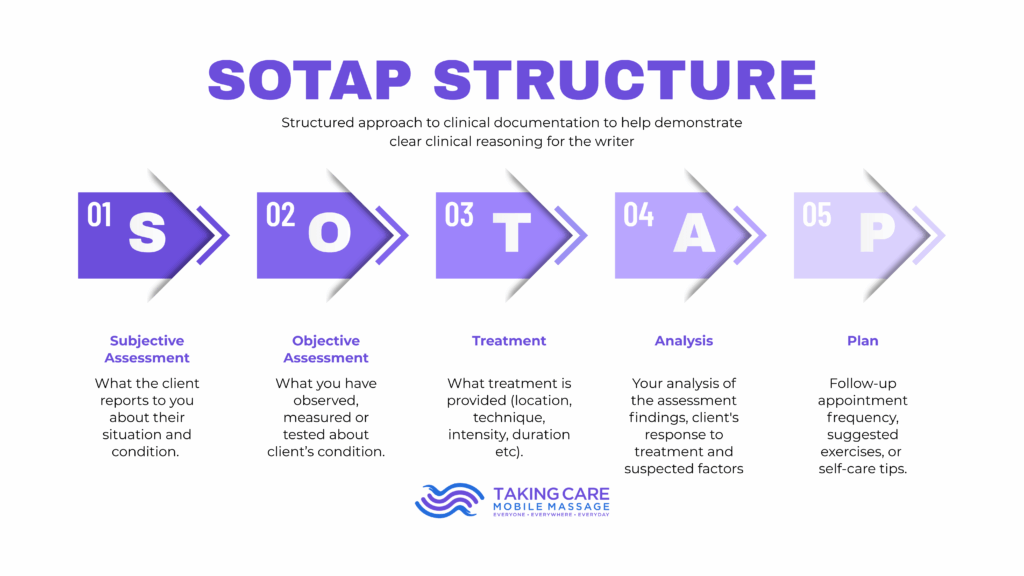
One of the most effective frameworks for achieving this clarity is the SOTAP structure. Whether you’re a new therapist or simply looking to improve the way you document sessions, SOTAP offers a simple and organised approach to writing notes that stand up to clinical, organisational, and auditing needs.
What Is SOTAP?
SOTAP is a structured documentation format designed to help clinicians present clear, logical, and consistent notes. It is a variation of the well-known SOAP format, adapted to better reflect the needs of therapists who work in mobile, community, and multidisciplinary settings.
The goal of SOTAP is straightforward: to help clinicians demonstrate clear clinical reasoning while maintaining concise, relevant documentation.
Why SOTAP Matters
In busy healthcare environments—especially mobile and community-based services—therapists often navigate diverse settings, varied client needs, and multi-provider communication. A structured format ensures:
-
Consistency: Every therapist documents in the same way.
-
Clarity: Notes are easy to read and follow, especially for others involved in the client’s care.
-
Accuracy: Key details aren’t missed during fast-paced days.
-
Professionalism: Documentation reflects high standards of care.
-
Clinical reasoning: Therapists showcase not just what they did, but why.
Breaking Down the SOTAP Structure
S – Subjective Assessment
This section includes what the client reports about their condition, goals, concerns, or changes since the previous session. It may include pain descriptions, functional limitations, or personal observations.
Example:
Client reports increased stiffness across the lower back following prolonged sitting at work.
O – Objective Assessment
This is what you have observed, measured, or tested during the session. Objective findings help support your clinical decisions and demonstrate progress over time.
Example:
Increased muscular tension noted in lumbar paraspinals. Limited trunk flexion observed.
T – Treatment
Here, you describe the treatment provided, including location, techniques used, intensity, duration, and any adjustments made.
Example:
Provided deep tissue massage to lumbar region (20 mins), trigger point release, and gentle stretching.
A – Analysis
This is your clinical interpretation of both subjective and objective findings. It shows your reasoning, connections between symptoms and assessments, and the significance of the changes observed.
Example:
Findings suggest muscular overuse related to posture. Client’s reported discomfort aligns with observed tension patterns.
P – Plan
This outlines next steps, including treatment recommendations, self-care advice, frequency of follow-ups, or referrals to other professionals.
Example:
Recommend weekly sessions for 2–3 weeks. Provided home stretching routine. Monitor progress; consider physiotherapy referral if no improvement.
The Impact of Using SOTAP in Practice
Implementing SOTAP ensures therapists maintain clarity and consistency while documenting complex clinical information. Over time, this leads to:
-
Stronger clinical decision-making
-
Better communication across teams
-
More effective and personalised treatment plans
-
Reduced documentation errors
-
Higher quality and continuity of care for clients
SOTAP is not just a structure—it’s a habit that strengthens your practice and supports the people you care for.